By Leading Edge Dental – Leesburg, FL
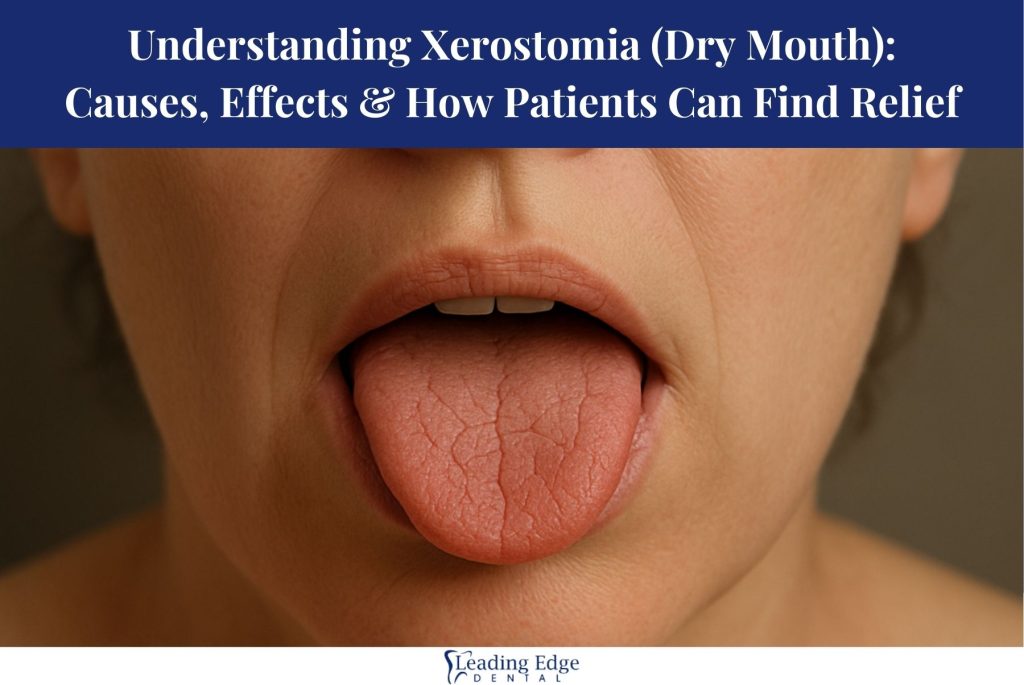
Dry mouth—clinically known as xerostomia—is far more common than most people realize. Whether it happens occasionally or persists daily, xerostomia can significantly impact comfort, speech, eating, and long-term oral health. At Leading Edge Dental, many patients come to us seeking relief, unaware that dry mouth may be a symptom of an underlying issue.
In this comprehensive guide, we’ll break down what causes dry mouth, how it affects your mouth and body, and what treatment options are available to help you feel better and protect your smile.
What Is Xerostomia (Dry Mouth)?
Xerostomia occurs when your salivary glands do not produce enough saliva to keep your mouth moist. Saliva is essential for:
- Neutralizing harmful acids
- Lubricating soft tissues
- Aiding digestion
- Preventing tooth decay
- Controlling bacteria and viruses
When saliva production decreases, discomfort and oral health issues can quickly follow.
Common Causes of Dry Mouth
1. Medications
Over 400 medications list dry mouth as a side effect, including:
- Blood pressure medications
- Antidepressants & anti-anxiety medications
- Antihistamines
- Pain medications
- Diuretics
This is the #1 cause of chronic dry mouth in adults.
2. Medical Conditions
Certain illnesses reduce saliva production, including:
- Diabetes
- Sjögren’s syndrome
- Parkinson’s disease
- Alzheimer’s disease
- Stroke recovery
- Autoimmune disorders
- Radiation treatments to the head or neck
3. Dehydration
Not drinking enough water, illness, vomiting, diarrhea, and excessive sweating can all cause temporary dry mouth.
4. Lifestyle Habits
Your daily habits may contribute to xerostomia:
- Smoking or using smokeless tobacco
- Alcohol use
- Mouth breathing
- Caffeine consumption
- Sleeping with your mouth open
5. Aging
Older adults are more susceptible due to:
- Natural changes to salivary glands
- Increased medication use
- Chronic health conditions
How Xerostomia Affects Oral Health
Without sufficient saliva, a variety of oral health problems can develop:
1. Increased Tooth Decay & Cavities
Saliva helps protect enamel. When it decreases, bacteria and acids cause cavities more quickly.
2. Gum Irritation & Gum Disease
Gums become irritated and prone to infection without moisture.
3. Difficulty Chewing, Swallowing & Speaking
Food may stick to the tongue or cheeks, and talking may feel uncomfortable.
4. Chronic Bad Breath
Bacteria thrive when the mouth is dry.
5. Higher Risk of Oral Thrush
A fungal infection called oral candidiasis becomes more common in dry environments.
6. Cracks, Burning & Mouth Sores
Soft tissues dry out, crack, and become more sensitive.
How Patients Can Find Relief from Dry Mouth
At Leading Edge Dental, we create personalized treatment plans based on the root cause of your dry mouth. Common treatment options include:
1. Hydration & At-Home Moisturizing Solutions
- Sip water throughout the day
- Use sugar-free gum or lozenges containing xylitol
- Avoid alcohol and caffeine
- Use alcohol-free mouthwash
- Sleep with a humidifier
2. Medication Review
If medications are causing dry mouth, we may collaborate with your physician to:
- Adjust the dosage
- Change the medication type
- Recommend supportive treatments
3. Saliva Stimulation & Substitutes
Over-the-counter and prescription options include:
- Saliva substitutes
- Oral moisturizers or gels
- Prescription medications (pilocarpine or cevimeline)
- Sugar-free lozenges
4. Dental Treatments
To protect your teeth from decay and damage, we may recommend:
- Prescription-strength fluoride toothpaste
- High-fluoride varnish
- Remineralizing treatments
- More frequent cleanings
5. Treating Underlying Medical Conditions
If diabetes, autoimmune conditions, or chronic diseases contribute to xerostomia, managing those conditions often helps reduce symptoms.
Dry Mouth Q&A: Expert Answers from Leading Edge Dental
Q: Is dry mouth something I should worry about?
A: Yes. Persistent dry mouth greatly increases your risk for cavities, gum disease, and infection. It’s important to identify the cause early.
Q: Can drinking more water fix my dry mouth?
A: Water helps relieve symptoms, but if saliva production is reduced due to medical conditions or medications, you may need additional treatment.
Q: What are the most common signs of dry mouth?
A:
- Sticky or thick saliva
- Bad breath
- Dry, cracked lips
- Burning sensation
- Trouble swallowing
- Frequent thirst
- Dry tongue or mouth sores
Q: Can dry mouth cause cavities even if I brush well?
A: Absolutely. Without saliva, cavity-causing bacteria multiply rapidly. Preventive treatments are very important.
Q: What toothpaste is best for dry mouth?
A: Non-whitening, fluoride-rich toothpaste formulated for sensitive mouths is generally best. We can recommend specific brands during your visit.
Q: Is dry mouth permanent?
A: It depends on the cause. If medications or dehydration cause it, symptoms may be temporary. Chronic conditions may require ongoing management.
Get Dry Mouth Relief at Leading Edge Dental
If you’re experiencing persistent dry mouth, we are here to help you find answers and lasting comfort. Our team will assess your symptoms, discuss possible causes, and create a personalized treatment plan.
Leading Edge Dental
📍 10601 US-441 Suite C-1B, Leesburg, FL 34788
📞 (352) 365-6442
🌐 Visit Our Website leadingdental.com Make an appointment leadingdental.com/appointments
Your oral health and comfort matter—let us help you feel your best again.
